93224-93226: Snag Extra Cash With These Tips
The catch is you have to make the request for your rightful dollars.
Here’s a piece of good news for you. As per the Medicare’s April update, three Holter monitor codes will get a slight boost in pay.
The change has an implementation date of April 4, 2011, and an effective date of Jan. 1, 2011. That means contractors have to be ready to comply with the change by April 4, but the change in practice expense relative value units (PE RVUs) is retroactive to Jan. 1 dates of service.
Medicare isn’t requiring contractors to search their files to adjust claims they have already paid (which is good news for any physician who reports a code seeing a fee decrease). But contractors do have to adjust claims if you bring them to their attention. Take a look at how many 93224-93227 services you provided from January to March to see if making the claim for the small increase in RVUs is worth your time.
93224: The PE RVUs for 93224 (External electrocardiographic recording up to 48 hours by continuous rhythm recording and storage; includes recording, scanning analysis with report, physician review and interpretation) will change from 2.30 to 2.53. That’s a difference of .23 RVUs. Multiply that by the 2011 conversion factor (33.9764), and you can expect roughly an additional $7.81 for this code. (Remember that geographic region will affect your fee, as well).
93225: For 93225 (…recording [includes connection, recording, and disconnection]), the PE RVUs only increase by .09, changing from 0.82 to 0.91. So the additional reimbursement should be roughly $3.06.
93226: You may see an additional $4.76 for 93226 (… scanning analysis with report). Its PE RVUs change from 1.21 to 1.35.
Swan-Ganz: If you ever report 93503 (Insertion and placement of flow directed catheter [e.g.,...

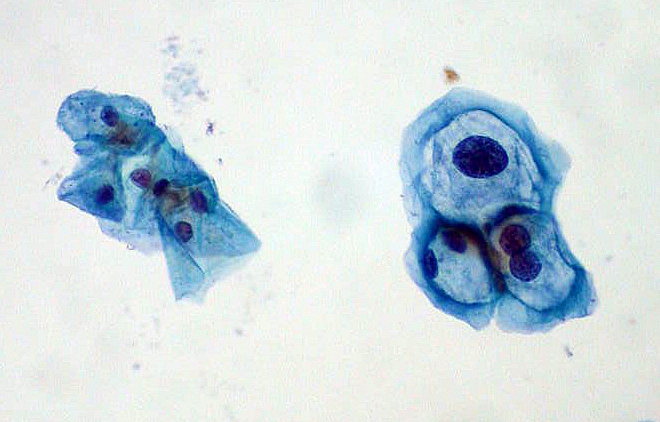 When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.

