No Correct Coding Initiative Bundle? Find Modifier Details in MPFS.
Question: Sometimes I cannot find my two-code pair in the CCI edits. How do I know which code would be considered a column 1 code and which would be considered a column 2 code, so that I could put my modifier on the correct code?
Answer: If the codes are not listed, the codes are not bundled per the Correct Coding Initiative (CCI). You would not need a CCI modifier, such as 25 (Significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service), 57 (Decision for surgery), or 59 (Distinct procedural service), to override the edit when appropriate.
A private payer could have a black box edit. You would need to check with a rep for a recommendation.
Watch out: Just because a code does not have a bundle in CCI does not mean a modifier is out of the picture. While you won’t need a CCI modifier to override the edit, you might need apayment modifier.
You can find Medicare’s other allowed modifiers for any given CPT code in the Medicare Physician Fee Schedule (MPFS). Columns Y-AC indicate if modifier 51 (Multiple procedure), 50 (Bilateral procedure), etc. apply.
To determine which code receives modifier 51, you need to know the code’s relative value units, which are also listed in the MPFS. Private payers may not adjust claim items in descending order as Medicare’s Outpatient Code Editor software does. If you append modifier 51 to a higher valued item, the private payer may apply the adjustment based on your coding, costing you payment. You should instead list the items in descending relative value order from highest to lowest. Append modifier 51 to the lower priced procedure as necessary. The insurer will then apply the typical 50 percent,...

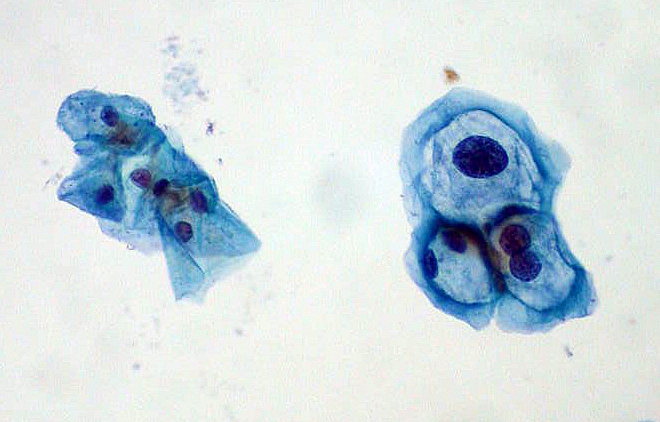 When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.


