Cyst Expression: I&D or Excision?
Question: Documentation reads, “The cyst was excised after performing a central incision directly on the cyst. All the material was expressed, then cyst capsule was removed completely and excised completely. Packing was performed.” Should I code the procedure as an I&D or an excision?
Answer: You should look at the pathology report and any further excision description to reach the correct code set. “Excision is defined as full thickness [through the dermis] removal of a lesion …,” according to CPT’s Excision-Benign Lesions guidelines. The documentation you provided does not indicate what tissue levels the excision involved. A cyst can be epidermal or sebaceous (706.2). A lesion that is removed from the epidermis (top skin layer) does not meet CPT’s excision definition.
The sebaceous gland extends through the dermis. Excision that deep would qualify for an excision code. An excision code (such as 11400, Excision, benign lesion including margins, except skin tag [unless listed elsewhere], trunk, arms or legs; excised diameter 0.5 cm or less) requires further documentation detailing the lesion’s morphology, size (including margins), and anatomical location. Without this information, the I&D code (10060, Incision and drainage of abscess [e.g., carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia]; simple or single) may be more appropriate. The physician made a cut to drain the cyst and then drained (expressed) all the material. The cyst capsule removal is part of the treatment of the I&D to prevent the blockage from reoccurring.
Take more coding challenges with Family Practice Coding Alert. Written by Jen Godreau, BA, CPC, CPEDC, content director of Supercoder.com, Family Practice Coding Alert, Volume 12, Number 6.

 Check out V13.65 for corrected congenital heart malformations.
Check out V13.65 for corrected congenital heart malformations.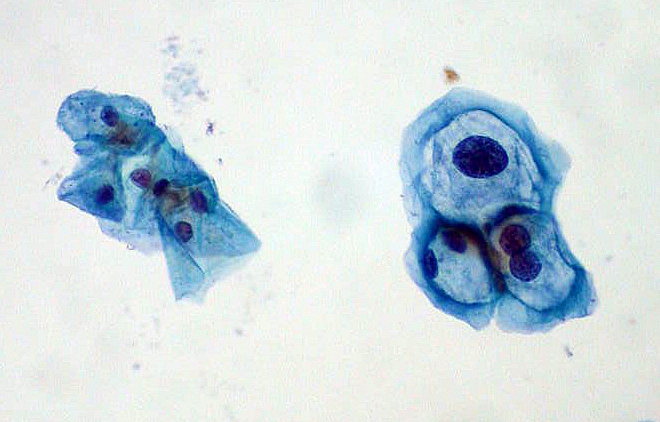 When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers. Say goodbye to form 4010A1 for ICD codes as well, starting in 2012.
Say goodbye to form 4010A1 for ICD codes as well, starting in 2012.