Hospital leaders are concerned that their organization’s clinical documentation and coding processes are vulnerable to errors that could result in lost or decreased revenue, according to a recent survey.
Consulting firm and technology vendor BESLER recently partnered with HIMSS Media to identify the greatest industry challenges and potential opportunities for revenue cycle improvement. They surveyed over 100 leaders within finance, revenue cycle, reimbursement, and health information management (HIM) departments at hospitals and acute-care facilities in October 2018.
The recently released survey results showed that 84 percent of respondents believe clinical documentation and coding are high or medium revenue cycle risk.
Hospital finance leaders were the most adamant that clinical documentation and coding presented significant revenue cycle challenges. Almost one-half of finance leaders chose clinical documentation and coding as their greatest revenue cycle vulnerability.
Although, the area was considered high or medium risk by over one-third of revenue cycle, reimbursement, and HIM leaders as well.
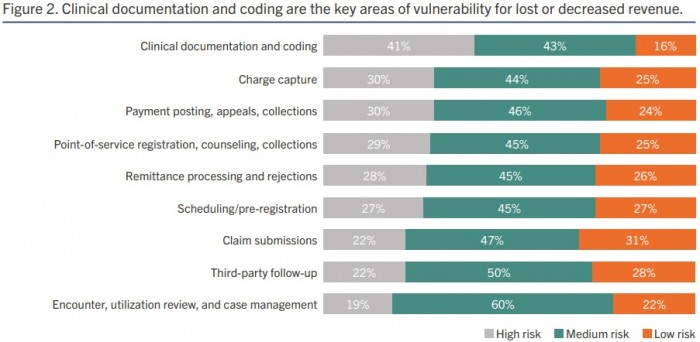
Source: BESLER and HIMSS Media
Clinical documentation and coding are creating revenue cycle vulnerabilities because solutions are not optimized for the diagnosis-related group (DRG) payment system, respondents shared. Only about one-third of hospital leaders said DRG optimization is a solved problem. In other words, the majority of hospital leaders (68 percent) do not think their solutions are equipped to manage DRG coding.
The DRG payment system has been around for over three decades. And major payers, including Medicare, use the payment system to determine lump-sum payments for hospitals that treat specific diagnoses.
While the payment system is not new, it is constantly evolving. Payers are attempting to get more specific about diagnoses to ensure hospitals are paid accurately for treating patients with certain conditions. The introduction of ICD-10 in 2015 is a prime example of how the industry has changed the DRG payment system.
But DRG changes are not ideal for providers. Hospitals find it difficult to follow and comply with constant DRG changes, and as a result, DRG coding accuracy has decreased. The report stated that the national benchmark for DRG assignment fell from 95 percent under ICD-9 to 72 percent in 2018.
Revenue cycle solutions, however, are optimized for inpatient coding and audits. Approximately 72 percent of respondents felt their technology is optimized for inpatient coding.
The survey also uncovered that respondents thought the accuracy of inpatient coding at their organizations was about the same as the industry benchmark.
Additionally, the majority of respondents (72 percent) agreed that their revenue cycle solutions are optimized for outpatient coding.
Opportunities to improve revenue cycle management technology remain. And poor coding integrity could result in the top two challenges hospitals face: claim denials (49 percent of respondents) and inaccurate reimbursements (47 percent of respondents).
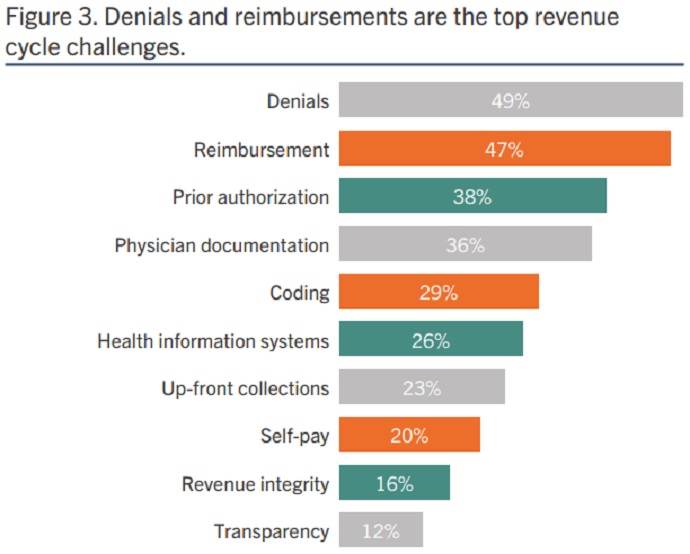
Source: BESLER and HIMSS Media
However, hospitals and health systems face significant obstacles with improving their mid-revenue cycle processes, including DRG coding and documentation. Chief among the challenges is a lack of budget. Nearly one-half of hospital leaders (49 percent) said budget constraints prevented their organization from improving DRG coding and documentation.
Nearly the same percentage of leaders also felt return on investment (ROI) was an obstacle. Forty-eight percent of respondents said difficulty proving ROI from investment stopped their organization from executing DRG optimization efforts.
Other obstacles to improving the mid-revenue cycle included:
- Competing projects (45 percent)
- Lack of staff/headcount to manage improvement efforts (38 percent)
- Lack of familiarly with solutions to address challenges (34 percent)
- Existing solutions already widely entrenched or accepted (32 percent)
- Overcoming internal perceptions that there is no need for improvement (30 percent)
Respondents identified a variety of challenges, but the survey also found a potential solution for hospitals and acute-care facilities. The survey showed that nearly half of respondents (47 percent) have created a revenue integrity program, which ensures organizations are being fully compliant with coding and billing practices while also achieving operational efficiency and legitimate reimbursement.
That means about 53 percent of hospitals still haven’t implemented a revenue integrity program.
About three-quarters of hospitals with revenue integrity programs reported improvements in net collections, increases in gross revenue capture, and/or reduction in compliance risk.
——————————————————
Photo courtesy of: RevCycle Intelligence
Originally Published On: RevCycle Intelligence
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro







