Today I would like to elaborate on recent remarks from Colleen Ejak regarding the 2025 Outpatient Prospective Payment System (OPPS) Proposed Rule regarding quality metrics and the inclusion of the social determinants of health (SDoH).
The Centers for Medicare & Medicaid Services (CMS) is expanding its SDoH initiatives for quality reporting from the inpatient setting, where they are currently in the mandatory reporting phase, to the outpatient setting, with a similarly staged rollout. The same measures and processes used in hospitals for inpatients 18 and older are proposed to be incorporated into the Hospital Outpatient Quality Reporting (OQR), Rural Emergency Hospital Quality Reporting (REHQR), and Ambulatory Surgical Center Quality Reporting (ASCQR) programs. Voluntary reporting will begin with the 2025 reporting period, followed by mandatory reporting in the 2026 reporting period/2028 payment or program determination.
Addressing Gaps in Care
CMS acknowledges that patients’ interactions with the healthcare system are often fragmented, and limited by the care setting. For instance, patients receiving care in Hospital Outpatient Departments (HOPDs), Rural Emergency Hospitals (REHs), or Ambulatory Surgical Centers (ASCs) may not have recently accessed care in acute-care hospitals or other facilities where SDoH screenings are already mandated. CMS’s proposed rule highlights that this gap can lead to missed opportunities to identify and address key social risk factors that significantly impact health outcomes. Notably, while the identification of social risk factors is included in this process and reporting, the systematic addressing of these factors is not yet standardized across many HOPDs, REHs, or ASCs.
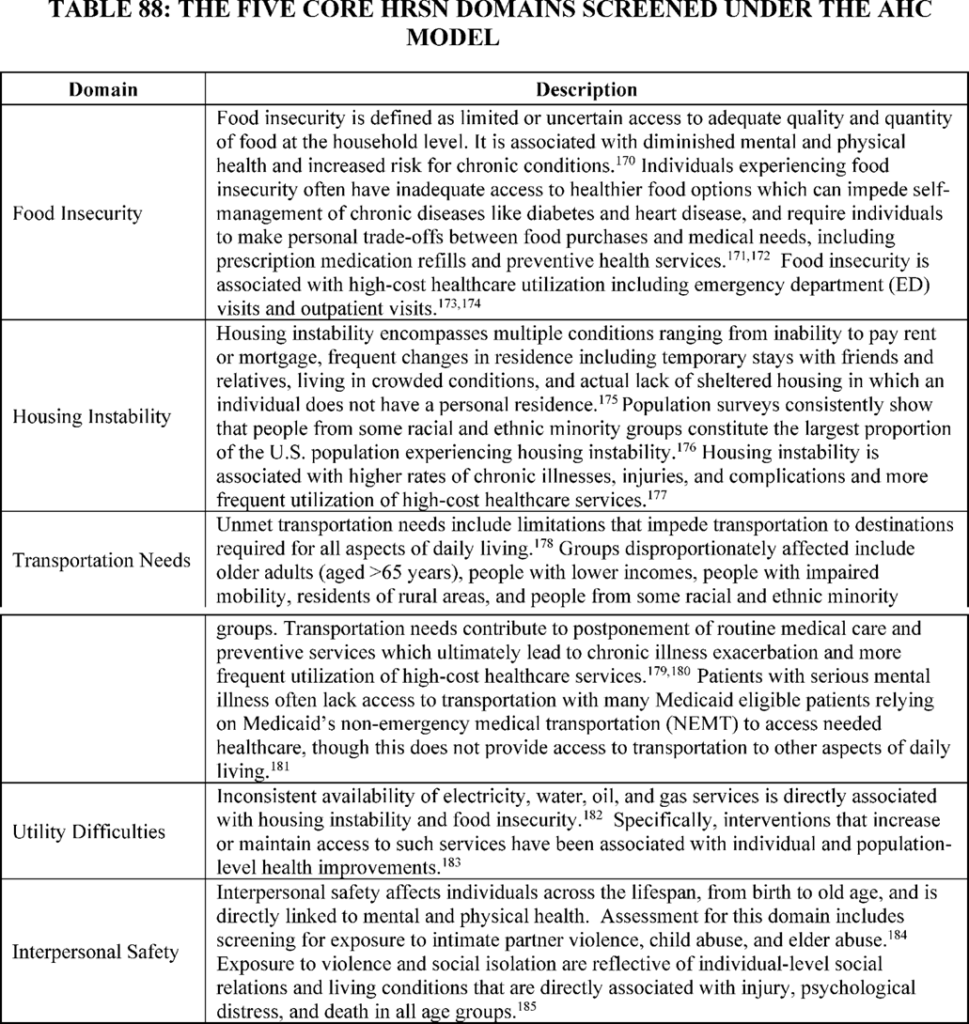
The expansion of SDoH screening to the outpatient setting aims to align and enhance the delivery of holistic care, ensuring that patients receive the necessary referrals and support to address critical needs in the five Health Related Social Needs domains, which include food insecurity, housing instability, transportation, utility challenges, and interpersonal safety.
Logistical Considerations for Implementation
Similar to the inpatient setting, the SDoH measure in outpatient settings will be calculated based on each outpatient encounter for patients 18 and older. Patients must be offered five specific Health-Related Social Needs (HRSN) domain questions related to personal safety, utilities, housing, transportation, and food insecurity during their care in a HOPD, REH, or ASC. The first measure will evaluate the proportion of patients who are offered the screening tool versus those who actually complete the questions. There are exclusions for those unable to complete or refusing to engage with the screening, which must be appropriately documented. CMS highly recommends that the tool be electronic.
Additionally, the Screen Positive Rate for SDoH measures will report on the percentage of patients who screen positive for one or more HRSNs. This data will be reported separately for each of the five HRSNs, allowing healthcare providers and policymakers to understand the prevalence of specific social risks in different care settings. The data will be reported annually. This will also provide continued data support for Z code capture.
Challenges in Operationalizing SDoH Screening
While this screening tool is a critical step towards addressing the SDoH on a broader scale, there are legitimate concerns regarding how to operationalize this process when a patient screens positive – and determining who will follow up on those needs. Currently, HOPD encounters include lab, imaging, radiology, bedded outpatients, same-day surgery, physician offices, and infusion departments, to name a few. It will be a massive undertaking to determine how these questions will be provided to patients and how appropriate follow-up will be conducted when a patient responds positively to one of them.
To prepare for this rollout, HOPDs, REHs, and ASCs should start discussing the following:
Mechanisms for incorporating SDoH Screening into the registration process: consider integrating these questions into your patient portal to be completed before or at the time of check-in. This will streamline data collection and quality reporting. HOPDs, REHs, and ASCs will need to assess all portals of entry to ensure that these questions are being provided for applicable patient encounters.
Plan for escalation and triage: develop a process for responding to positive SDoH screenings. Something we have learned from responding on the inpatient side to numerous positive screens is to include a question that asks if the patient is already receiving assistance for each need. The questionnaire should also include a question as to whether the patient would like to speak to someone further about their response. If the answer is no, follow-up may not be required, and this should be documented as such. If the answer is yes, determine if the issue can be addressed via a phone call at a later date, or if someone should be available to address the need during the visit. Immediate action should be taken for concerns related to personal safety, while issues related to housing, utilities, food, and transportation could be routed to appropriate teams for timely but non-immediate follow-up. This approach could involve partnerships with community organizations, ambulatory care management departments, post-acute resource centers, or telehealth/phone-call outreach services, likely some type of case management outreach support.
This measure represents both a challenge and an opportunity. It challenges clinicians to integrate SDoH screening into routine care processes, ensuring that all patients are assessed for social risks that may impact their health. At the same time, it offers an opportunity to enhance patient care by addressing the root causes of health disparities and expanding Z code capture, which can improve patient care outcomes.
——————————————————
Originally Published On: ICD10 Monitor
Photo courtesy of: ICD10 Monitor
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro







