The Centers for Medicare & Medicaid Services (CMS) intends to align its Medicare plans, including Part D prescription plans, with the Centers for Disease Control and Prevention (CDC) opioid prescribing guidelines. On January 5, 2017, the agency released a statement justifying this action. Because of “the growing body of evidence on the risks of misuse [of opioid medication], and the Administration’s commitment to combating the opioid epidemic, CMS is outlining our agency’s strategy and the array of actions underway to address the national opioid misuse epidemic,” noted the agency.
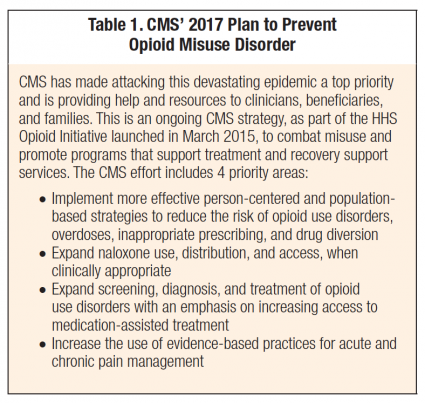
According to CMS, “The Medicare population has among the highest and fastest-growing rates of diagnosed opioid use disorder, currently at more than 6 of every 1,000 beneficiaries. For Medicaid beneficiaries, the prevalence of diagnosed opioid use disorder is even higher, at 8.7 per 1,000, a figure estimated to be over 10 times higher than in populations who receive coverage under private insurance companies.”2 In its announcement, the CMS outlined its plan to combat opioid misuse (Table 1).
As everyone involved with pain management now knows, the major controversial point in the CDC guidelines is the suggestion that primary care physicians should avoid increasing opioid dosages to 90 morphine milligram equivalents (MME).1 The 90 MME standard, as written in the guidelines, applies to primary, not specialty, care, and calls for evaluation and justification for dosage above this level—it is not a “ceiling” or maximal dosage.
Unfortunately, some third-party payers and biased parties claim this is the maximal dosage of opioids that can be safely prescribed. As I noted in my January/February Editor’s Memo: a survey of 1,978 chronic pain patients found that 68% said their opioid medication had been decreased or stopped since the CDC adopted its prescribing guidelines.3 In addition, 45% of respondents were warned by their doctor that additional decreases will be necessary. Most striking, just over 50% said they had considered suicide as a way to end their pain.3
CMS was ready to use 90 MME as a “ceiling” or maximal dose but recently changed its policy after hearing from affected patients, families, and physicians.4 This commonsense change is a commendable humanitarian gesture.5 Until recently, the CMS planned to recommend 90 MME to be a maximal dose without justification to exceed this level. If a dose exceeds this level, Medicare insurers are expected to impose a “soft edit” that would automatically block the prescription from being filled until the edit is overridden by a pharmacist. Under the previous CMS proposal, insurance companies could also impose a “hard edit” that could not be overridden on prescriptions that exceed 200 MME. The new policy allows a pharmacist to override the 200 MME edit if the prescribing physician shows that this high opioid dosage is medically necessary.
CMS reports there were a “significant number of comments” from the public that encouraged this policy change. The CDC estimates that about 11.2% of the adult population has chronic pain.1 This translates to some 25 million people, of which a considerable number require high-dose opioids. Patients and families of patients who require high-dose opioids are organizing and becoming a potent advocacy force. Physicians should encourage patients to join the advocacy movement. If a segment of our society needs high-dose opioids, they will have to speak out or poor pain control will adversely affect their quality of life and function.
CMS also reports some facts to back up what we practitioners knew was occurring in recent years. Opioid prescriptions per capita have been decreasing for several years—since even before the movement to enact guidelines with dosage limits. CMS reports that between 2011 and 2015, Part D enrollees decreased high-dose opioid prescriptions (120 MME for 90 consecutive days) by 47%. Even without guidelines, opioid prescriptions per capita have continued to decrease as practitioners have opted to prescribe a greater number of prescriptions for opioid alternatives and potentiators.
The new CMS policy is extremely important. At last someone in the federal government acknowledges that some severe chronic pain patients require over 200 MME a day. Let’s all take advantage of this “de facto” declaration and educate all parties that there are occasionally chronic pain outliers who require over 200 MME.
——————————————————
Photo courtesy of: Practical Pain Management
Originally Published On: Practical Pain Management
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro