As it was billed and touted, ICD-10-CM/PCS gives medical personnel vastly expanded powers of specificity when diagnosing diseases and other health issues. Yet that greatly enhanced specificity comes with a price tag—a transition period that some observers believed could be messy and disruptive.
As physicians and other healthcare workers learned to adapt to the system, healthcare professionals feared productivity, and revenue, would plummet sharply.
The transition had been much feared for years, and efforts to implement it in the U.S. had been stalled. The World Health Organization released the final version of ICD-10 in 1992, and the U.S. clinical modification was available as early as 1999. Finally, federal agencies set Oct. 1, 2015, as the first day for use of the new code set to submit claims to Medicare.
Many were worried, even though much of the industry had been preparing for the transition for months, even years. Some even went so far as to call ICD-10 the “Y2K” of medical coding.
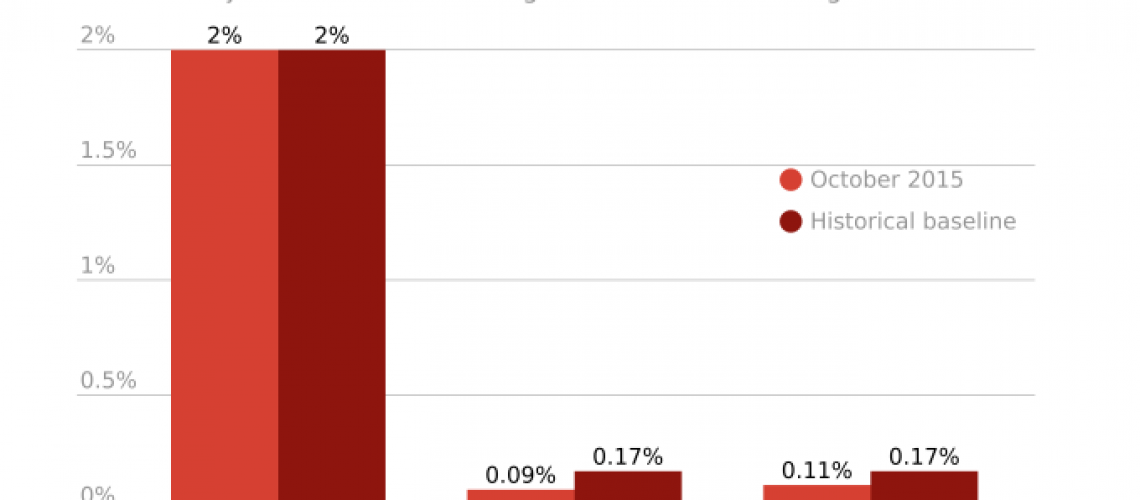
Early reports gathered by the Centers for Medicare and Medicaid Services suggested that the transition had gone well, with no spikes in rejections of Medicare claims submitted during October 2015. Now that we are more than four months into the transition, were these ICD-10 fears more hype than reality?
Early reports gathered by the Centers for Medicare and Medicaid Services suggested that the transition had gone well, with no spikes in rejections of Medicare claims submitted during October 2015. Now that we are more than four months into the transition, were these ICD-10 fears more hype than reality?
By gathering field reports and provisional data, we’ve come to the following early conclusions about the transition:
- Not everyone was ready. This was due, in part, to previous delays in the ICD-10 implementation. In the spring 2014, Congress intervened to push the implementation date back a year, to Oct. 1, 2015. And throughout 2015, some providers were expecting another delay in the transition, and that reduced the urgency of some to prepare. While the transition was relatively smooth from an information technology perspective, productivity impacts ranging from 30 to 50 percent have been realized for organizations that didn’t adequately prepare. Some HIM departments have offset productivity impacts by incurring overtime or employing contract staff.
- Ingrained behavior of physicians still must be changed. Hospital personnel are still adapting to the pressure to provide more documentation, a sometimes tall order in a hectic hospital environment. Increased documentation is necessary because coders need more specificity to determine the right ICD-10 code.
- ICD-10 isn’t being used to its fullest capabilities yet. According to preliminary data gathered from select clients, fewer than 10 percent of the 140,000 ICD-10 classification codes are being used.
- The learning curve is significant. That same data shows that more than a quarter of assigned ICD-10-CM diagnosis codes include the term “unspecified.”
- Denials have increased – but it is still early. While there have been a few issues on the reimbursement side, most have been relatively minor. However, productivity has taken a significant hit for many healthcare systems, and it’s too early to tell if productivity will ever rebound to pre-ICD-10 levels. Denials will increase once the ICD-10 “grace period” ends and approvals must meet more stringent standards.
Some caution that ICD-10 interpretation issues may still loom as 12,000 hospitals and other providers adapt to the system simultaneously. Complicating matters is the system by which such questions are addressed – coding advice from federal agencies is scheduled to be released only on a quarterly basis. HIM professionals have described this process as “laborious” and not designed to offer timely guidance.
The last major hurdle to a successful transition will involve changing longstanding behavior and work habits, as physicians are asked to provide more thorough documentation. Organizations are evaluating the need to reinforce clinical documentation improvement initiatives, and strengthen quality assurance and revenue integrity functions to improve coding accuracy. This will enable organizations to adapt to changes that may come from payers later down the road.
Once coders and healthcare professionals get fully up to speed, the specificity gains offered by ICD-10 will have come at a relatively minor cost in terms of patient care and successful reimbursement procedures.
——————————————————
Photo courtesy of: Health Data Management
Originally Published On: Health Data Management
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro