As a wary nation emerges from lockdown, front-line healthcare workers know that an uncertain future remains ahead.
One of the most stressful things about the COVID-19 pandemic is how fast things are changing. Emergency medicine has always been a stressful career, and the nature of the work, combined with the weekend/night/holiday shifts, have created significant strain on my life and relationships over the years. It is also a job that puts you at risk for assault, injury, or even death.
Over the years, I have had my life threatened by those distressed over an unexpected outcome, or the addicted, over an opioid prescription. During the 2009 swine flu pandemic, I thought I might die when I contracted it and had to see patients anyway due to short staffing, but I didn’t.
To work in the ED during this pandemic, you accept that you are taking a real (albeit small) chance with your life. But I can’t recall seeing any other time in my career when things changed so fast.
Overall, my region has fared better than other regions of the country, and my native West Virginia is moving towards relaxing social distancing measures aligned with the data model from the University of Washington. In my clinical practice, I am seeing fewer COVID/suspected COVID patients than in previous weeks. I always focus on the suspected patients, because that is all you can say about them when they first come through your door.
Testing has changed from a 5-7-day turnaround to a 24-hour turnaround where I have been working, and that has lifted the burden on how long you have to isolate someone in the hospital or quarantine them at home. In the first weeks of the pandemic, we thought that 90 percent of COVID-19 patients would have a fever, and to preserve PPE,
I would save my solitary N-95 mask for febrile patients. Based on the Journal of the American Medical Association (JAMA) study from Northwell last week, only 30 percent of these patients present with fever. So I have changed my approach again, donning full PPE, all day, every day until it falls apart, and then I get a new mask from a secret stash that a colleague told me about.
We are continuing to see true emergency cases and slightly higher volumes of behavioral health patients who are decompensating from our collective anxiety. In yet another change, we are starting to see more less-acute cases, as patients are either responding to messaging about lifting restrictions or are suffering from over a month without primary care. I have seen a couple of cases that became surgical emergencies directly related to the delay of their elective cases.
I think we will continue to see things shift as we start to open things back up. We will see cases rise and fall in certain areas, and I am sure some states will go back to social distancing. Given the low association with fever, the number of asymptomatic carriers, and the estimated 10-fold more than those tested who are infected among us, I think that we will wax and wane with this for the next year.
But to be clear, social distancing has worked. It has bought us time: time to learn about the disease, time to learn about what treatments work, and time to work on a vaccine. It has also given me time to see that, from a fatality rate, this first wave is going to be about three times as bad as the annual flu season. That is, until something else changes.
——————————————————
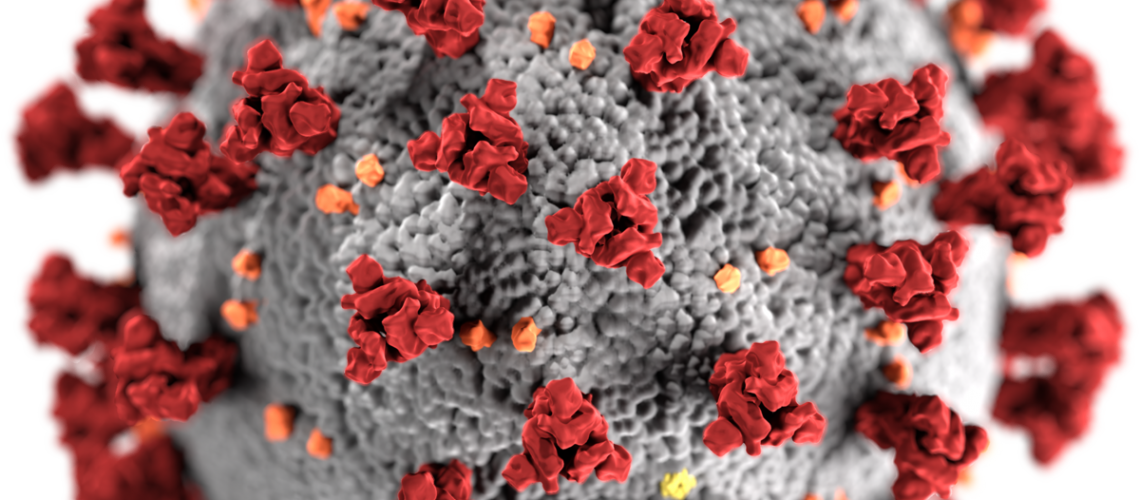
Photo courtesy of: RAC Monitor
Originally Published On: RAC Monitor
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro