Too little attention is paid to documentation, coding, and billing in many medical practices. For patients, documentation simply means that your doctor is providing an account of your visit in your medical record. However, documentation and coding can affect revenue, quality of care, and possibly expose clinicians to legal consequences.
Too often doctors and other healthcare providers (PAs, NPs, etc.) cruise through their documentation and coding training, giving short shrift to the nuances of this key aspect of care delivery. In fact, many medical practices offer no formal training in the use of Current Procedural Terminology (CPT©) codes and Internal Classification of Diseases (ICD) codes. In these instances, despite such inadequate preparation, doctors simply begin seeing patients and documenting medical visits in the electronic health record (EHR). I’m sure that most clinicians would rather just see patients than bother with the billing component of care delivery, which includes charting the patient’s condition, selecting the correct CPT© code of the 10,294 that are available, and choosing the right diagnosis codes out of the 68,000 that are available. The difficulties involved are further complicated by the hierarchical condition category (HCC), which involves assigning risk scores to patients. Add to these complexities the effects that coding may have on compensation, and you can see that the process is rife with potential problems. For instance, many physicians, especially those working in health systems, are paid for their delivery of care on the basis of a work relative value unit (wRVU), a measure determined by Medicare.
Accurate documentation helps provide a baseline of the cost of patient care, and it can affect profitability. It’s essential that clinicians accurately document all of their work so that they not only provide a complete medical record of delivery of care but also receive full and fair reimbursement for their services. Accurate coding can also offer some protection during audits. On the other hand, inaccurate coding can have unintended and deleterious consequences.
What Is Coding?
Coding involves charting and documenting the service provided during a patient’s visit. When you enter your doctor’s office, he or she may provide the services required for a low-intensity office visit and may document having provided Level 2 service. The problem arises when the doctor, whether intentionally or unintentionally, provides Level 2 service butdocuments that a Level 4 service was provided, or documents that Level 2 service was provided but bills for Level 4 service. Such disparities leave doctors open to charges of having overbilled for a visit, overbilling that risks fines and, in the worst cases, jail time.
wRVUs and Compensation
Medicare assesses medical work on the basis of wRVUs. Figure 1 below shows wRVUs for five codes used to document new patient visits in 2019. After your first visit to a new doctor, the doctor may have billed your insurance company using one of these codes. These five codes range in meaning from least comprehensive medical service (99201 or Level 1) to most comprehensive medical service (99205 or Level 5). In theory, more work is required for a Level 5 visit than for a Level 1 visit. Medicare pays doctors for the level of service provided. So if a 99201 service was provided, a doctor is paid less than if a 99203 service was provided. If a 99201 service was provided but a 99203 service was documented and submitted, the doctor has overbilled. Today In: Innovation
Figure 1
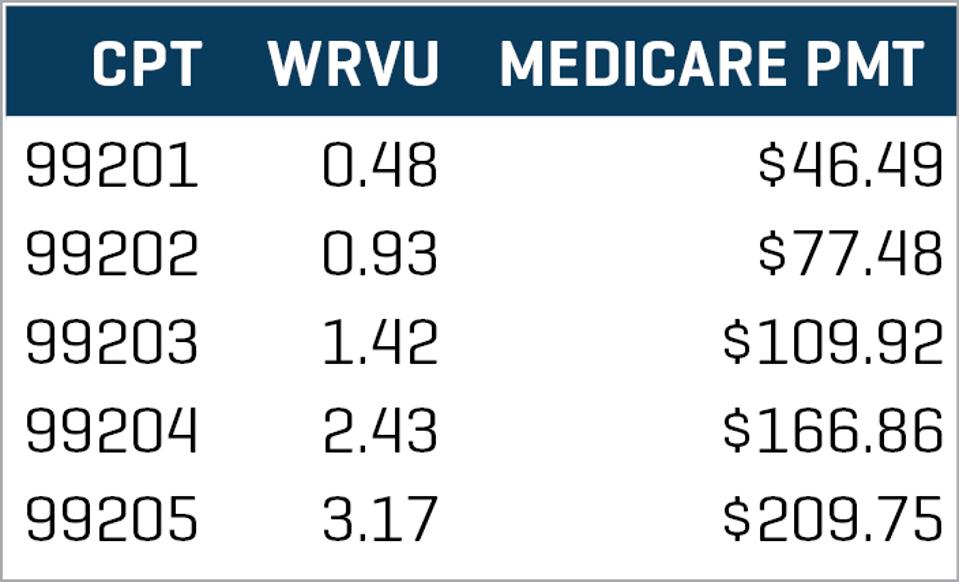
Good documentation is critical not only for the sake of protecting doctors and other medical practitioners from the legal risk that attends incorrect coding and overbilling but also for the sake of providing accurate documentation of care and good quality of care.
Some physicians are paid in part as a result of the wRVUs they produce. Figure 2 illustrates a simple example.
Figure 2
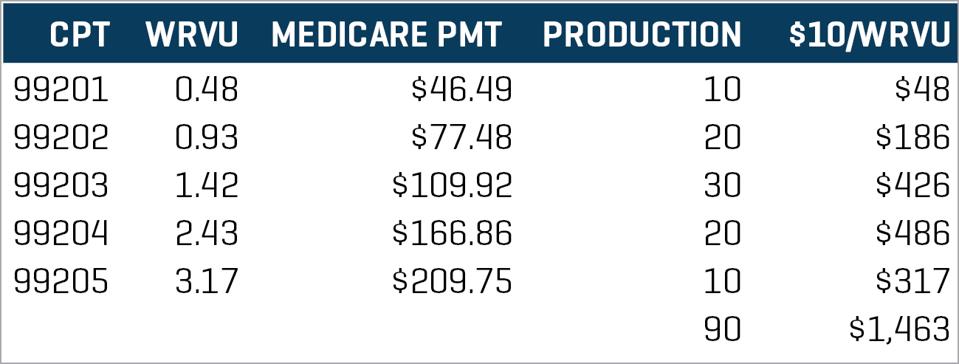
Figure 2 shows the charges made by a doctor who sees 90 patients and generates $1,463 in pay at a rate of compensation of $10 per wRVU. But what if this doctor should have had a normal or bell-shaped coding distribution (as in Figure 1) butinstead had billed everything as a Level 3, Level 4, or Level 5?
Figure 3 illustrates the case of Dr. X, who sees 90 patients but bills mostly for Levels 3 to 5. In so doing, Dr. X has increased his or her pay by $569 for a total of $2,032, a 39% increase!
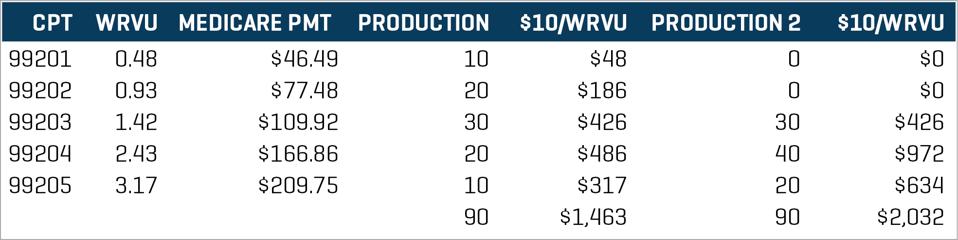
Now, this isn’t to suggest that Dr. X is necessarily doing anything wrong. Maybe this doctor has sicker patients requiring more work and effort. Of course, Dr. X has documented all this in order to justify each instance of charging for Level 3, Level 4, or Level 5.
Let us stipulate that Dr. X is indeed seeing sicker patients and that the coding is accurate. Although a doctor may be able to pass a coding audit with flying colors, other questions also may arise. For instance, was it really possible to see these 90 patients? Are there enough hours in the day? In other words, let us stipulate that the coding is accurate and that Dr. X passes a hospital-based coding audit. The documentation is apparently appropriate and the billing accurate. Obviously, regardless of how “accurately” the doctor has documented and billed, he or she could not have seen 90 sick patients in one day. So although documentation may be rock-solid in many respects, other considerations must also be attended to when assessing documentation, coding, and billing as a whole.
Medical practices and health systems can help to ensure high-quality coding and documentation—and therefore more accurate reimbursement and better quality of care—by:
· Ensuring that visits are properly documented and coded by providing education that includes refresher training at periodic intervals (e.g., annual training on standards, changes in codes, etc.)
· When a clinician has had significant errors, ensuring proper remedial follow-up for the clinician with a goal of improving coding accuracy
· Ensuring that, even when doctors pass coding audits, their work is still assessed in terms of volume coding within given time frames, places of service (e.g., surgery versus clinic time), etc.
· Rinsing and repeating….often
Documentation and coding of visits affects medical practices in many ways. If improperly done, they can be a dangerously weak link in medical practice. If aggressively and proactively managed, however, they reduce audit risk, reduce the risk of malpractice suits, and enable effective management of revenue and expenses.
——————————————————
Photo courtesy of: Forbes
Originally Published On: Forbes
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro