 A delay in requiring all providers of medical care to use a new health-records and billing system to describe treatments is giving small medical offices major headaches.
A delay in requiring all providers of medical care to use a new health-records and billing system to describe treatments is giving small medical offices major headaches.
Billing is a big task for small medical practices. It takes time away from patient care and requires extra staff. A federal mandate requiring doctors to adopt a new set of billing codes by Oct. 1, 2014, was about to make everything more complicated.
Then, in late March, Congress bowed to pressure from such groups as the American Medical Association and the Medical Society of the State of New York to delay the changeover.
Physicians, along with hospitals, other health care providers and insurers, now have at least until Oct. 1, 2015—and possibly longer—to convert to the system, which uses a new set of codes for labeling ailments and treatments. Known as the ICD-10, for International Classification of Diseases, the system is far more precise and detailed than its current version, the ICD-9. Even though the ICD-10 system has been used internationally since 1992, U.S. medical organizations fought for the delay because of the cost of the change.
But now that it’s here, not everyone is happy.
“The delay is unfortunate and will be costly,” said Sandra Sperry, a self-described “ICD-10 transition specialist” who is chief executive of SPS and Associates, a Brooklyn-based health technology consulting firm.
Better record-keeping
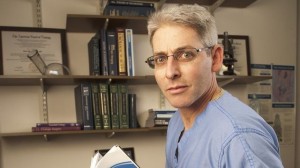
Many physicians agree, said Dr. David Weiner, a urologist who is part of a four-physician practice on Manhattan’s Upper West Side. So far, the changeover has mostly cost his practice time.
“I’ve gone to several training sessions; we’ve all been aware ICD-10 was coming, and we felt pressured to be prepared,” he said, noting that there is a lot to learn. “The old system had about 13,000 codes, and this one will have about 68,000.”
At AdvantEdge, a national physician practice consulting firm in Warren, N.J., Bill Gilbert, vice president for marketing, said his company has worked with physicians, including about 500 doctors in the New York metro area, since 2011 to train their staffs in using ICD-10. “To delay it for a year is very disruptive, costs us money and costs our clients money,” Mr. Gilbert said. His own firm was putting its coders through a 20-week ICD-10 training program when the delay was announced. The company will likely slow that timetable, he said.
Many physicians, coders and insurance companies have already spent time and money buying software and training people on the new systems. According to a February 2014 study commissioned by the AMA, the average cost to small practices will run from $57,000 to $226,000. In pushing unsuccessfully to reject a delay, the Centers for Medicaid & Medicare Services, a federal agency, estimated the additional cost of a reprieve at more than $1 billion nationally.
The coming switch has already cost Dr. Christine Doucet both time and money. She owns Patchogue (L.I.) Family Medical Care, a group with three doctors and three physician assistants. The practice has purchased a software update that lets its team use either ICD-10 or ICD-9 codes for now.
“I’ve been going to conferences on how to use it [ICD-10], and now we’ll have to have refresher courses,” Dr. Doucet said.
ICD-10 gives everyone—the patient, the providers and the payers—a much better medical record, she and others agreed.
Reimbursement risks
“If I treat a patient for an earache now, all I have to write is one three-digit code,” she said, but under the new system that code will run out four more decimal places. The first new digit could designate whether it was the right or left ear; the second might show whether there was fluid in the ear; the third would note whether antibiotics were prescribed; and a fourth could be used to show whether the earache was a recurring problem.
But physicians fear payment denials.
“If you leave some of those decimal spaces as zeros, you would get paid a lot less—typically $12 for an earache instead of $42,” Dr. Doucet said.
If the wrong code was entered, the claim would be completely rejected, with no reimbursement.
“Everyone’s been warning us to set aside enough money to cover three months of operating expenses because a lot of claims are going to be rejected, and we won’t have money coming in,” she said. “Some practices were planning on taking out bank loans for that because most of us just don’t have that kind of money.”
That was the main reason the state medical society fought for the delay, but Dr. Weiner said the switchover was unavoidable. “That train’s coming down the track, and you can’t stop it,” he said.
——————————————————
Prepare For The Medical Coding Certification Exam Here!
Originally published on: Crain’s New York Business
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1






