 Maximize 11040-11044 pay with modifier 51.
Maximize 11040-11044 pay with modifier 51.
In most cases, your practice won’t report debridement separate from wound repair codes. But when exceptions arise, follow these three tips to choose the appropriate wound repair code.
If you’re considering reporting debridement separate from a wound closure, make sure your physician’s notes clearly document that the wound was contaminated and required saline or other substances or instrumentation to cleanse and debride the wound.
Don’t miss: If you report a debridement code with your wound closure codes, append modifier 59 (Distinct procedural service) to the debridement code. This informs the payer that you recognize that debridement is generally bundled into wound repair, but that clinical circumstances required the physician to perform debridement as a separate service.
1. Look for Wound Repair With the Debridement
CPT specifies that you may also report debridement codes independently of repair codes when the physician removes large amounts of devitalized or contaminated tissue or when the physician performs debridement without immediate primary repair of a wound, notes Pamela Biffle, CPC, CPC-I, CCS-P, CHCC, CHCO, owner of PB Healthcare Consulting and Education Inc. in Watauga, Texas.
The physician may clean debris from the wound without repairing the wound because it was either not deep enough to require repair or the physician delayed the repair due to an extenuating circumstance.
In the case in which the dermatologist excises a lesion, debridement is included in the procedure. However, when the dermatologist only performs debridement or performs the debridement in addition to the wound repair, such as the case when a wound is excessively dirty or contaminated with debris, you would also code the debridement code with the wound repair/excision code, appending modifier 51 (Multiple procedures) for the multiple procedure.
Example: A patient returns to the dermatologist several days after a chemical...

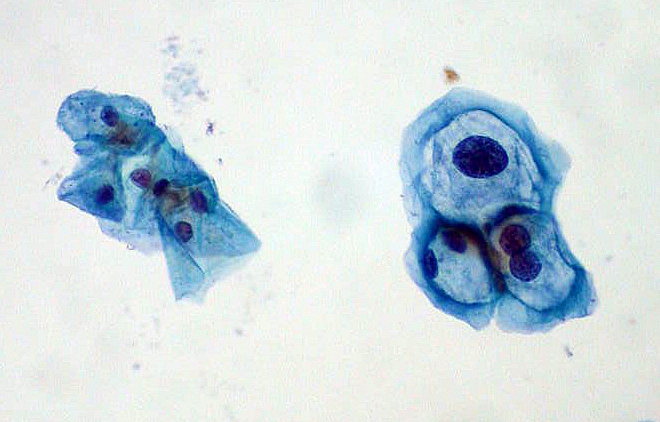 When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.
When a patient returns to your office for a repeat Pap smear, you’ve got to weigh your options of E/M and specimen handling codes, as well as diagnosis codes. Take this challenge to see how you fare and prevent payment from slipping through your fingers.