The COVID-19 pandemic has driven digital transformation across healthcare at an unprecedented speed.
Telemedicine has emerged as an essential tool for maintaining patient/doctor communication during the crisis, enabling clinicians and hospitals to build new models for care provision for the post-coronavirus future.
The coronavirus pandemic is a challenging situation for healthcare systems. In some regions of the world the crisis is easing down, while in other areas it is still stretching healthcare to the limits. Many providers are simply trying to stay on top of it from one spike to the next.
The need for communication methods to provide services such as monitoring and consultations – without the patient having to be physically present or spend hours in a waiting room – became clear virtually overnight. And this rapid evolution was quickly accepted by many providers and patients as the ‘new norm’.
Invention not required
The focus of early telemedicine solutions was to improve care for heart failure patients and reduce hospital stays, as well as to manage the treatment of chronic diseases remotely. At the heart of eHealth adoption is the understanding that a patient’s acceptance of digital services depends on their state of health and the belief that they can make a difference to how it evolves, alongside the practical requirement for mobile device ownership – such as smartphones and wearables.
The COVID-19 pandemic revealed the extent to which this framework already existed. “The requisite infrastructure for connectivity is widely available at both ends of the clinical encounter, most readily through the smart phone,” wrote the authors of a guest editorial for TELEMEDICINE and e-HEALTH. “Most healthcare systems in private and public sectors have already deployed electronic health records, thereby ensuring continuity of care for their patients.”1
The impact of the pandemic on one hospital’s telemedicine strategy was revealed in a study led by researchers from NYU Grossman School of Medicine, which focused on the experiences of NYU Langone Health. According to the study, between March 2nd and April 14th 2020, virtual urgent care visits grew by 683% and non-urgent virtual care visits grew by 4,345% in response to COVID-19. The medical facility had already established centralized virtual health ecosystems that included a patient app offering a central point of access for all healthcare needs.2
The digital journey
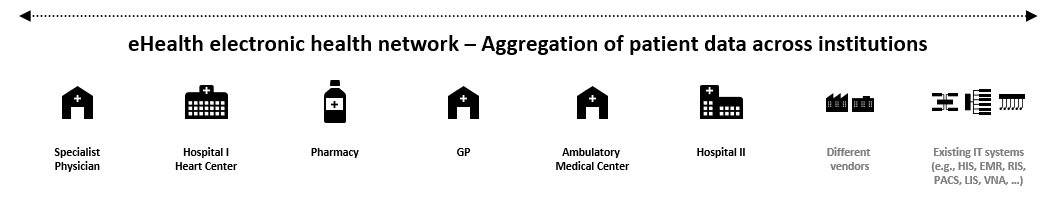
Experiences like this show that bringing together all important patient data helps to create a better overall picture of a patient’s health. Aggregating these data can help make predictions about outcomes. And a safe, secure infrastructure helps minimize the separation of patient data, reducing record keeping costs and resources.
Now, the most frequently analyzed data come from Electronic Health Records (EHRs). Due to advances in natural language processing and the growing popularity of wearable health tracking devices, web and social media data as well as biometric and sensor data also play an increasingly important role.
This means EHR and other health data can be used to develop personalized care plans, which in turn will improve the whole healthcare system. Today, big data is being captured and exploited more effectively – for example, with the collection of everyday health data via the internet of medical things (IOMT) – meaning that immediate responses become possible at every point of a patient journey.
As the authors of the TELEMEDICINE and e-HEALTH editorial observed, telemedicine offers capabilities to utilize rapidly developing scientific and technological advances within networks that transcend geography.3
eHealth connections
Before the pandemic rose to a global crisis, Siemens Healthineers had already been creating and further developing eHealth solutions for more than a decade. These solutions were originally introduced to break down data silos and enable interoperability among departments, within IDNs (integrated healthcare delivery networks in a dedicated region) or among healthcare providers in a certain region.
Countries with notable eHealth solutions up and running include Denmark, Austria, Switzerland and Germany. From EHRs to automated and paperless prescriptions, these systems are digitalizing the healthcare system in a revolutionary way.
For example, in Austria, Siemens Healthineers has partnered with the national drive to make EHRs available for all citizens. More than 140 institutions are already using the ELGA (electronic health record, locally called “elektronische Gesundheitsakte”), and 5 million citizens are now on the system.4
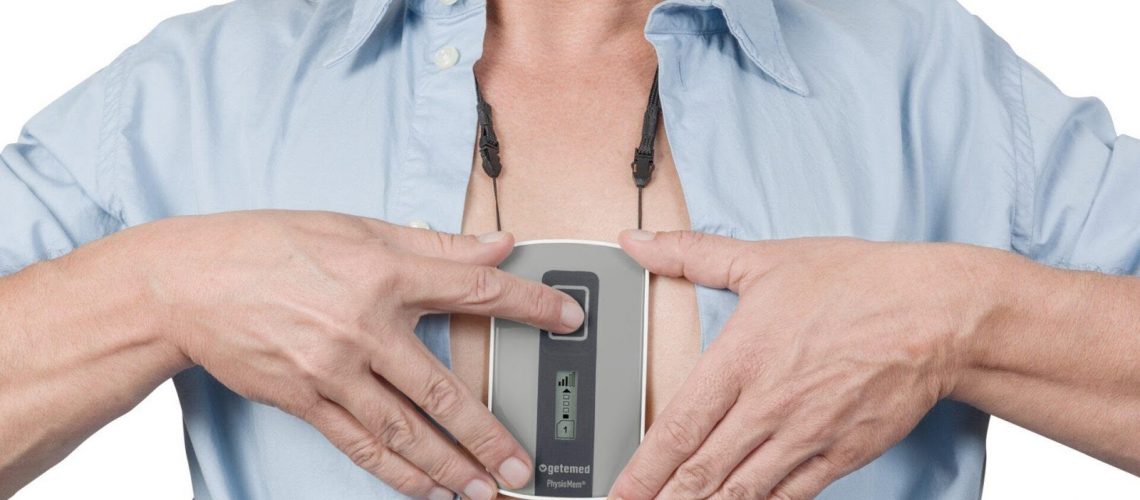
Another telemedicine project benefiting patients is “HerzConnect” in the German town of Bad Oeynhausen, which may assist physicians in preventing heart failure and reducing hospital stays, and has already been adopted by several health insurance companies.
Data security included
The rush to build telemedicine applications in response to COVID-19 has perhaps inevitably raised fears that this speed could compromise data security. So, there are clear advantages in choosing an established system that is built on many years of knowledge and expertise in this area. For example, patient consent has always been a key aspect of Siemens Healthineers’ mobile health solutions.
An automatic save function for documentation and immediate data access are combined with an unambiguous patient identification by name, gender, date of birth and patient ID. The patient is given opt-out flexibility for selected content and documents from the start. And of course, compliance with security standards, national and international data security policies, and with interoperability standards, is also built in.5
Patient involvement
teamplay myCare Companion allows healthcare providers to design their own telemedicine programs and flexibly adapt the underlying technology to their needs. teamplay myCare Companion basically consists of two components: an intuitive smartphone app for patients and a special workstation for medical care providers. Patients use the app to report their health status, wellness, the medications they’re taking, and their vital parameters to the nursing staff. Among other things, the program helps employees quickly identify patients whose state of health may have worsened. The attending doctors can then decide whether a scheduled hospital visit should be moved forward or if more intensive remote medical care would be beneficial.67
Video consultation is another eHealth benefit that has come into its own during the pandemic, reducing the time patients spend physically in medical facilities to see their doctor, and minimizing the risk of infection. Siemens Healthineers ‘Virtual Visit’ solution has been released and being deployed at first customer sites.

By enabling patients and supporting clinicians to manage cases at home, the solution will provide an infrastructure to alleviate pressure on essential facilities. This is a good example of how telemedicine might represent the future of managing increased demands on the healthcare system in a postCOVID-19 climate, giving safer control to doctors and nurses over managing the vital medical resources that have been under such severe pressure during the pandemic. 8
Agent of transformation
It is clearer than ever that the future of healthcare depends on digital transformation, making data interoperable for the benefit of the patient and enabling personalized healthcare. It will enable patients to be involved in their own wellbeing as the topic of COVID-19 recedes. During the ongoing crisis, it has in some cases shown to be a potential agent for increasing patient outcomes while helping the medical facility to stay within its limit of resources and capacity. In future, eHealth will also help to reduce costs for healthcare providers and patients, while meeting the expectations and demands of patient-centric healthcare delivery without compromising on either outcome or data security.
——————————————————
Photo courtesy of: Becker’s Hospital Review
Originally Published On: Becker’s Hospital Review
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro