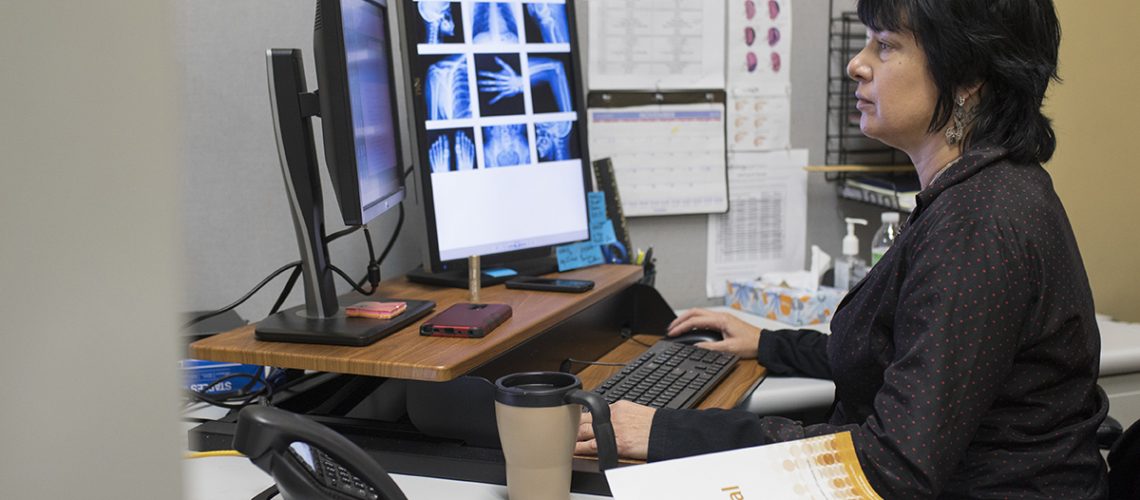
After two years of following a doctor around the office as a medical assistant, Raina Diaz was ready for a change.
“I wanted to be part of the back end of the medical field,” says Diaz, 47, of St. Petersburg, Florida.
She enrolled at her local state college, where she learned that becoming a medical coder could be a way of staying in her field without being on the front lines. Now as a certified coder she analyses clinical statements and assigns standard codes using a classification system.
“I like the solitude, keeping busy reading the reports and figuring everything out,” says Diaz, who specializes in radiology.
According to 2016 data from the Bureau of Labor and Statistics, the demand for medical coders is expected to rise 13% by 2026 due to an aging population that will require medical care. The average median salary of a medical coder in 2017 was $39,180.
With demand in this occupation increasing, we spoke with professionals working in the field and the classroom about how to become a medical coder.
First, What Does a Medical Coder Do?
Before you receive a bill from a hospital or a doctor’s office, a medical coder processes your medical chart.
The chart contains your diagnosis, treatment plan and other relevant information. It’s the job of a medical coder to review those records and put the relevant information into a coded classification system, says Kengia Sabree, the health information technology academic chairwoman at St. Petersburg College.
“The purpose of coding is to help reflect the severity of illness,” she says. “So if you’re not coding correctly, you’re not necessarily capturing how sick the patient is or all of the resources the hospital is using to care for the patient.”
Once all the information is coded, it’s sent to the billing department so the hospital or doctor’s practice can bill the patient or their insurance company.
What Kind of Credentials Do I Need?
The two organizations that provide coding credentials are the American Health Information Management Association (AHIMA) and the American Academy of Professional Coders (AAPC).
Each specializes in different areas of coding: AHIMA focuses on inpatient coding used in hospitals, while AAPC focuses on outpatient coding for physicians’ offices or clinics.
If you’re interested in following the hospital track, look into obtaining the Certified Coding Associate (CCA) entry-level credential through AHIMA. But if working in clinics or outpatient centers sounds like a better fit, then go for the Certified Professional Coder (CPC) entry-level credential with AAPC.
Obtaining the CCA can demonstrate that you know the basics of coding, but it may not open up all hospital job opportunities. The Certified Coding Specialist credential (CCS) is a more advanced certification that requires on-the-job coding experience before you’re eligible to take it.
“If you want to advance in a hospital, you’ll need a CCS after one year in the field,” Sabree says.
Do I Need a College Degree for Medical Coding?
Sabree says aspiring medical coders have two options to consider when they begin their studies. They can take the core classes needed to prepare for the CCA exam, or they can earn a Health Information Technology associate of science degree — the parent degree for medical coding.
Students who want to get into the workforce as quickly as possible should pursue a medical coding certificate, Sabree says. This certificate program includes essential classes like anatomy and physiology, medical terminology, intro to health information management, coding classes and field experience.
While that may be the quickest way into the field, Sabree encourages her students to stay and get their two-year associate degree. If the coder ever decides to go into management or move up the ranks in a hospital, they will need to obtain the Registered Health Information Technician (RHIT) certification.
“It may be a little bit easier to earn the associate’s degree in the beginning to prevent you from having to go back to school,” she says.
Plus, any extra experience and schooling in the beginning can give your resume a boost when applying for those competitive entry-level jobs.
“It’s a very difficult profession to be in without some good educational background and experience,” said Melissa Myrick, director of health information management at BayCare Health Systems in Clearwater, Florida. “We turn away coders quite often based on not having enough education and background for our positions.”
Both Sabree and Myrick warn potential coders to research coding programs thoroughly before enrolling and make sure they’re accredited.
“We see so many billboards and flyers about becoming a medical coder in 10 weeks or six months,” Sabree say. “Those are what I call the fly-by-night programs. There’s something that you always have to keep in mind wherever you go: [The schools] have to be programmatically accredited.”
Check to see if the school or certificate program is recognized by AHIMA or AAPC. You can check your school’s accreditation through CAHIIM here or AAPC here.
How to Become a Medical Coder – Who Is Actually Employed
Once you have your degree and credentials, it’s time to start applying for jobs. Sabree tells her students to look for positions such as “coding apprenticeships,” “coding level one” and “coding trainee.”
“Those are the coding positions that are geared toward people without having the experience, and then the facility typically guides you from there,” she says. Some medical facilities give exams to figure out which types of coding are best for the new coder.
X-rays, electrocardiograms and emergency room coding are typical entry-level coding gigs. Myrick says most coders will need to start there before moving to more complex specialties.
In recent years, the option to work from home has become more available. Sabree says some places are hiring people to work remotely right away, while others require coders to meet productivity goals before giving them that option.
Who is best suited for this line of work? Lifelong learners who are interested in medicine.
A Word About Automation
Like many professions, computer automation is disrupting the medical coding field. Computer-assisted coding already does some of the work that humans used to do. But not all of it, and that’s key.
Simply put, computer-assisted coding, or CAC, automatically generates medical codes directly from clinical documentation. And with the advent of electronic medical records, where every piece of a patient’s information is contained in a unique field rather than scribbled in a doctor’s handwriting, it’s easy to see how computers can do that work.
But there’s always the possibility for error, and that’s where human eyes and scrutiny and judgment still have an important role to play. In that light, think of CAC as something that can assist professional coders rather than replace them.
In addition, as computers become more able to complete low-level coding tasks, that leaves more room at the top.
AAPC addressed this in a February 2019 blog post.
“As we move into a more artificial intelligence environment, higher level coding skills will be needed, such as clinical documentation improvement, auditing and education. And those who are developing and maintaining CAC systems will always need coders to continually improve and challenge the system,” the post said.
——————————————————
Photo courtesy of: The Penny Hoarder
Originally Published On: The Penny Hoarder
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro