By combining traditional medical data with self-reported SDOH data, the codes trigger referrals to social and government services to address people’s unique needs.
KEY TAKEAWAYS
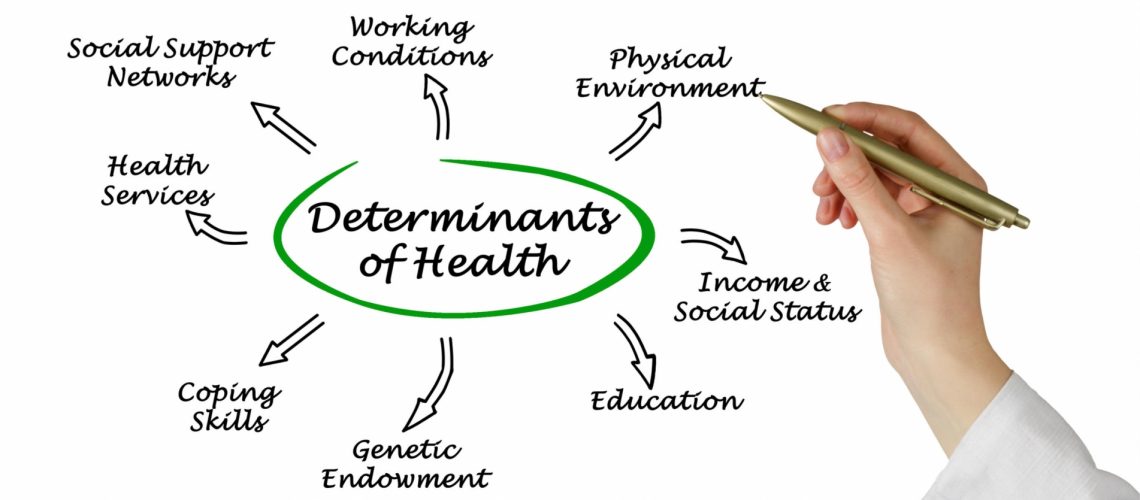
Increasingly, payers, providers, and state and federal governments are acknowledging the critical role that SDOH plays in proactive care delivery.
The collaborative wants to standardize how SDOH data are collected, processed and used in patients’ care plans, noting that there exists no organized method to capture that data.
UnitedHealthcare, and the American Medical Association have launched a collaboration to create nearly two dozen ICD-10 codes to better incorporate social determinants of health into healthcare delivery.
The collaborative wants to standardize how SDOH such as food, housing, transportation, employment, and financial means are collected, processed and used in patients’ care plans, noting that there exists no consistent, organized method to capture that data.
By combining traditional medical data with self-reported SDOH data, the codes trigger referrals to social and government services to address people’s unique needs, connecting them directly to local and national resources in their communities, the collaborative said in a media release.
Through this collaboration, UnitedHealthcare and the AMA’s Integrated Health Model Initiative are supporting the creation of nearly two dozen new ICD-10 codes related to SDOH.
“The collaboration reinforces the importance of social and environmental factors in patient care, and will shape IHMI’s efforts to support clinical decisions with useful and valid data to achieve broad improvements in health and greater health equity,” said Tom Giannulli, MD, CMIO at IHMI.
Using its data model, UnitedHealthcare said it has made more than 700,000 social-service referrals for enrollees in its Medicare Advantage plans since 2017.
Increasingly, payers, providers, and state and federal governments are acknowledging the critical role that SDOH plays in proactive care delivery.
In 2016, CMS amended the Medicaid managed care rule to prompt Medicaid MCOs to help patients with nonmedical expenses that were considered crucial to achieving health outcomes and cutting costs.
Under the CMS Accountable Health Communities Initiative, many Medicaid MCOs assess patients’ unmet social needs, including housing instability, food insecurity, utility needs, interpersonal violence, and transportation requirements.
An increasing number of states are requiring Medicaid MCOs to address social determinants of health as part of contractual agreements. In New York, The Empire State’s Value Based Payment Roadmap requires MCOs to offer startup funds for partners in Value Based Payment agreements who are conducting social determinant of health interventions.
“The collaboration reinforces the importance of social and environmental factors in patient care, and will shape IHMI’s efforts to support clinical decisions with useful and valid data to achieve broad improvements in health and greater health equity.”
——————————————————
Photo courtesy of: Health Leaders Media
Originally Published On: Health Leaders Media
Follow Medical Coding Pro on Twitter: www.Twitter.com/CodingPro1
Like Us On Facebook: www.Facebook.com/MedicalCodingPro